Pathfinder’s contributions to professionalization of the community health workforce in Africa

Much of the impact Pathfinder has had over the past several decades is owed to our invaluable local partners—the community health workers we work with every day. They have reached many millions of people with information about contraception, pregnancy, and delivery, and myriad other health-related and reproductive health-related issues—changing and saving lives.
Community health workers are trusted by their communities, as confidantes, mentors, and civil servants. They are the ultimate bridge between communities and the health system, and they are a critical part of improving health and advancing rights. Through our programs across the African continent, we’ve worked with our government partners to support and invest heavily in “professionalizing” the community health workforce, ensuring community health workers have the resources and skills they need to do their jobs well and earn the recognition, renumeration, and respect they deserve.
Our support and investments toward professionalization have included numerous trainings on the technical skills necessary to provide contraceptive counseling that adheres to the values of voluntary and informed choice; use of new technologies; provision of contraceptive methods at community level; as well as information and referrals related to pregnancy and delivery, HIV and other sexually transmitted infections, cervical cancer prevention and treatment, safe abortion care, and other issues and diseases, such as malaria, nutrition, and gender-based violence. We have worked with community health workers to lead group discussions on sensitive topics related to sexual and reproductive health and rights, shifting beliefs and norms in support of greater gender equity and access to health care.
Expanding and increasing coverage of services that can be provided by community health workers in the community could avert 2.3 million maternal and child deaths per year.
Black RE, Taylor CE, Arole S, et al. Comprehensive review of the evidence regarding the effectiveness of community-based primary health care in improving maternal, neonatal and child health: 8. summary and recommendations of the Expert Panel. J Glob Health. 2017;7(1):010908. doi:10.7189/jogh.07.010908
This work continues today and is ever more relevant as we face a continued global pandemic, climate crisis, and multiple protracted conflicts that are significantly increasing the burden of disease and risk of death, particularly in many African countries. Given these enormous challenges, we continue to make our partnerships with community health workers a priority and advocate for investing in their professionalization within the health workforce. In the following sections, we highlight some illustrative examples of our work that over the past several years have improved health outcomes through close partnership with community health workers across Africa.

Burundi: Community Health Workers Address Broad Array of Health Issues
Anne Marie Ntahombaye, a community-based distribution agent, visits her client, Victoire Mibuka, at her home. Photo: Jean Sacha Barikumutima
Over the past year, 410 community health workers learned how to provide Sayana Press (DMPA-SC) at community level, and 2,493 community health workers received trained on Integrated Community Case Management of illnesses among children under 5, with a specific focus on malaria.
As they are in many other countries, community health workers serve as the first point of contact between the community and the health system in Burundi. They are expected to provide a wide range of services including information that contributes to the prevention and management of illnesses, distribution of health commodities, and identification and referral of people to health facilities for treatment. The government pays its community health workers through a performance-based financing system, where each community health worker receives money in proportion to services provided. Pathfinder’s US Agency for International Development (USAID)-funded Tubiteho program and European Union-funded HealthNet TPO program, offer enhanced systems for support, training, and supervision—broadening the types of services community health workers provide and ensuring they have the support necessary to do so.
To date, every pregnant woman goes for antenatal consultation early, before they reach three months. We have even been equipped with rapid pregnancy tests and trained to help doubting women know their status for sure and in entire confidentiality, thus inducing them to seen services confidently.
Julienne Niyibigira, a community health worker supported by Pathfinder in Burundi
One of the reasons community health workers often can’t work to full capacity in Burundi is the reality of overstretched health providers who do not have the energy to adequately supervise and train community health workers. Yet community health workers have the potential to take on many of the tasks now assumed by health providers, saving them time and effort. Pathfinder has worked with a select number of providers to offer enhanced supervision through simple, low-cost strategies like sharing with community health workers the names and addresses of people that have missed appointments for vaccinations, antenatal care visits, and family planning, so that the community health workers can follow-up without having to review records and analyze the data themselves; broadening the services offered during each home visit; and pre-verification of data before submission to the national health information system. Our trainings for community health workers have included a focus on data collection and management, and interventions proven to curb the number of mothers and children falling ill and dying from preventable causes, such as community management of common childhood illnesses including malaria, pneumonia, and diarrhea and access to the community-based distribution of contraceptives.

Democratic Republic of the Congo (DRC): Community-Based Distributors Expand Access to Family Planning and Teach Women to Self-Inject Sayana Press
Agnesse Milolo Tshimanga, a community-based distributor from Bilomba Health Zone to Kasai Central, visits a couple for a family planning session. Photo: Aimé Tshibanda Muteba
- From 2018-2020, community-based distributors contributed to 13,303 women, for the first time, using Sayana Press (DMPA-SC).
- From 2020-2021 during the COVID-19 pandemic, 171,636 women in three provinces, for the first time, used a method of family planning.1
Injectable contraceptives are a popular contraceptive method across many African countries, but many women do not live near health facilities where injectables, like DMPA-SC, are offered. Through our USAID-funded Evidence to Action project, from 2018-2020, Pathfinder held trainings with nurse supervisors who, in turn, cascaded trainings on self-injection to community-based distributors, covering 15 health zones in 3 of DRC’s 26 provinces. Community-based distributors supplied DMPA-SC to women in rural areas and assisted them with learning how to self-inject—giving them increased and sustained autonomy over their reproductive decisions, particularly during the COVID-19 pandemic when access to services have been even more limited.
Since then, through Pathfinder’s Clinton Health Access Initiative-Funded Catalytic Opportunity Fund, Pathfinder has supported the Ministry of Health to finalize national guidelines on self-injection. The guidelines have been applied in more than half of health zones, covering 15 out of 26 of DRC’s provinces and providing 11 million women of reproductive age access to DMPA-SC.
Training community-based distributors on DMPA-SC self-injection offered a wider contraceptive method mix to more women and showed that a competent, non-clinical community health workforce has been able to safely provide DMPA-SC and teach women to self-inject. Community-based distributors remain an essential part of filling the human resource shortages that characterize DRC’s health system, where there is less than 1 physician for every 1,000 people.

Niger: Community Health Workers Provide Implants and Community-Based Distributors Provide DMPA-SC
Zara Lamine, a community health worker, gives Implanon to Abdourahamane Kadidja Hassane, mother of 5 children, in Dosso, Niger. Photo: Tagaza Djibo
- Community health workers administered Implanon NXT to 3,756 women from January 2020 to August of 2021.
- Community-based distributors injected 14,923 women with DMPA-SC and referred 16,567 women to health posts and health centers for other contraceptive methods over a three-year period ending in March 2022.
In Niger, less than 12% of women of reproductive age are using a modern contraceptive method largely due to cultural norms that inhibit the use of contraception and lack of information and services reaching women, particularly in rural areas. Task shifting is one of the most effective strategies being applied to increase access to and use of contraception.
To account for the inaccessibility of contraceptive methods, particularly clinical methods like implants, in Zinder, Tahoua, and Dosso, Pathfinder worked with local health system partners to train 405 community health workers to offer implant insertions and removals at health huts, which provide basic primary health services in rural areas. Pathfinder, working with the Ministry of Health, also trained 280 community-based distributors to inject DMPA-SC, raise awareness about contraception, and refer women to health posts and health centers for a full range of contraceptive methods.
In advance of these trainings, Pathfinder, through its IMPACT program, participated in advocacy efforts to ensure government policies allowed for community health workers to provide implants, and the necessary medical equipment and supplies would be available. We then organized trainings led by health providers, and regional- and district-level trainers that allowed community health workers to learn about insertion and removal techniques and to spend two days in practicum. Following the trainings, trainers conducted regular supervision to ensure safety and efficacy, and services were continually monitored. This approach has allowed women in the some of the most remote areas of Niger to access implants and DMPA-SC—which were out of reach previously.

Uganda: Foundational Work on the National Community Health Worker Program
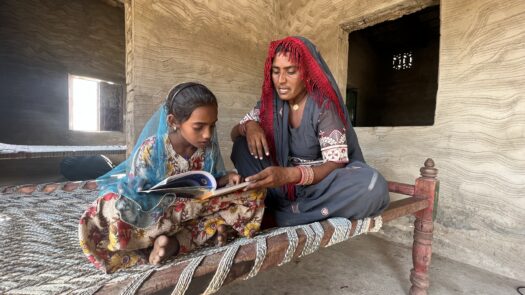
Jamida Kyamumi, a member of a Village Health Team, conducts a health education session. Photo: Lovington Kambugu
$2.17 million allotted to train community health extension workers (CHEWs) and national community CHEW curriculum developed.
The foundation for professionalizing the community health workforce lies in the national policies that govern their services and budgets that give them resources to do their important work. In Uganda, from 2016-2019, Pathfinder worked closely with partners and the support of the USAID and the Ugandan government in strengthening its community health worker program by adding community health extension workers (CHEWs) (full-time, paid community health works with formal, standardized training) to existing Village Health Teams (VHT)—volunteer, part-time workers who operate at community level. Pathfinder played a significant role in conducting a VHT assessment, which identified gaps in the community health program that might inhibit the government from achieving its goals related to curbing maternal and child mortalities, reducing HIV transmission, and increasing contraceptive use. This assessment was used to inform a national curriculum for CHEWs.
With UNICEF, we brought together stakeholders, including representatives from the Ministry of Health, to develop a community health roadmap and support the development of a CHEW policy. We then supported the Ministry of Health to select CHEW candidates from 13 pilot districts and prepare for training 1,640 CHEWs. In terms of resourcing the policy, we brought together the Ministry of Health with a national financing alliance, which designated more than US$2 million for training CHEWs, and contributed to research on financial and non-financial incentives that could be used to motivate CHEWs.
Resourcing and supporting CHEWs remains a national priority in Uganda today because of these intentional efforts to join stakeholders and use evidence-based information for advocacy toward strengthening the community health system. The government is still looking at ways to strengthen community-health facility linkages and ensure services reach the last mile.
The Future of Africa Relies on the Community Health Workforce
The examples described in this blog are just some of the numerous efforts Pathfinder undertakes each day to support our community health workforce partners around the world. The goal of universal health coverage and challenges of growing disease burdens, climate change-induced health issues, and working under the constraints of significant human resource shortages across health systems will never be possible without fully resourcing the community health workforce.